Table of Contents
Mpox is making the rounds in conversations everywhere—newsfeeds, social media, you name it. With so much chatter, it’s easy to feel lost in the noise. So, here’s our take on the situation: what’s actually going on with Mpox, how it’s playing out in places like India, Globally, and, most importantly, what you can do to keep yourself and your loved ones safe. Let’s cut through the clutter and get straight to the stuff that matters.
The First Case of Monkeypox Death in India, 2024
Mpox, formerly known as Monkeypox, has emerged as a significant global health concern, with a worrying uptick in cases worldwide. India, which had previously managed to contain localized outbreaks, is now under increased scrutiny.
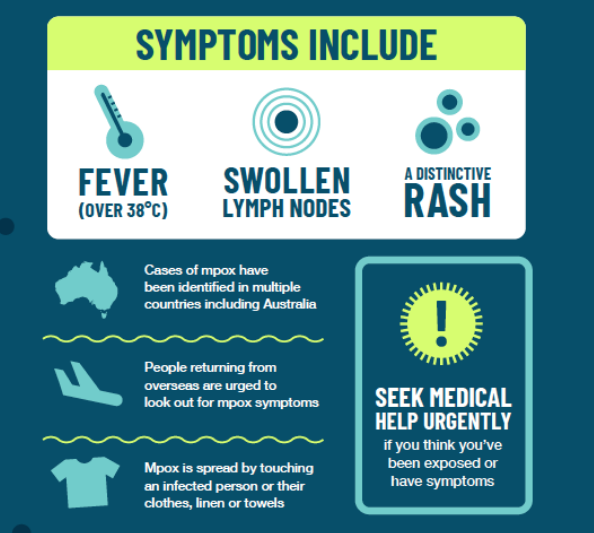
India reported its first Mpox-related death in the southern state of Kerala. A 22-year-old man who had recently returned from the United Arab Emirates passed away shortly after his arrival. He had tested positive for the virus abroad, but after his arrival in Kerala, his condition rapidly deteriorated. He exhibited symptoms like fever and swollen lymph nodes, but the absence of visible rashes initially led doctors to overlook Mpox. It was only after his death that the National Institute of Virology confirmed the virus.
In response, Kerala’s state government quickly formed a high-level committee to investigate the medical case and the delay in seeking treatment. Twenty close contacts, including his family and acquaintances, have been isolated as a precaution. Authorities are also reaching out to fellow passengers from his flight, though so far, there’s no cause for widespread alarm regarding their exposure.

India continues to navigate Mpox outbreaks in 2024, with the most recent case reported in Kerala this March. Since the initial surge of cases in 2022, the country has recorded 30 confirmed instances of Mpox. Despite the rising numbers globally, health officials in India have managed to keep the situation under control, and a major outbreak seems unlikely. The Indian government has been proactive, implementing stringent monitoring and control measures to prevent further spread.
Global Mpox Outbreaks
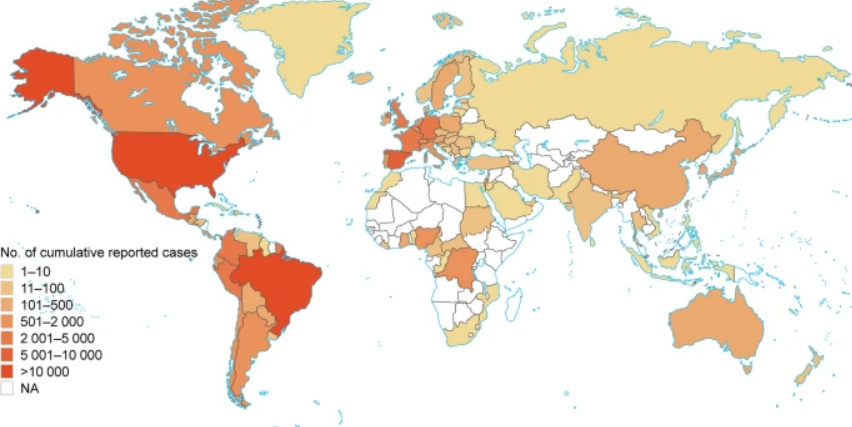
The global spread of Mpox shows a clear pattern of regional variation, with the Americas and Europe bearing the brunt of the outbreak. The United States, Brazil, and several European countries like Spain, France, and the United Kingdom have reported over 10,000 cumulative cases, making these regions the most heavily impacted. The Democratic Republic of the Congo (DRC) is also facing its worst Mpox outbreak yet, with a staggering 160% increase in cases and a 19% rise in deaths compared to last year.
Latin America, Brazil and Colombia continue to see high case numbers, while Africa and the Middle East report moderate levels, with countries like Nigeria and Saudi Arabia registering between 101 and 500 cases. Meanwhile, Asia and Oceania, including India and Australia, are seeing fewer cases within the same range, hinting at a more contained spread. Large parts of Africa, Asia, and Oceania show either minimal cases or lack sufficient data, which might indicate successful containment, underreporting, or smaller outbreaks.
Amid this varied global landscape, health authorities remain on high alert, focusing on early detection and rapid response to any new cases. Public health campaigns have ramped up, aiming to raise awareness about symptoms, transmission, and prevention. Efforts are also underway to enhance surveillance systems, improve diagnostic capabilities, and ensure that healthcare facilities are equipped to manage potential cases. The goal is to keep the public informed and prepared, all while preventing the situation from escalating further.
What is Mpox?
Mpox is a viral zoonotic infection, meaning it’s a disease that can jump from animals to humans. It’s caused by the Mpoxvirus, a name that reflects its history—though the virus was first discovered in monkeys back in 1958, its primary reservoirs are actually rodents like rope squirrels, tree squirrels, Gambian pouched rats, and dormice. The first known human case was recorded in 1970 in the Democratic Republic of Congo.
Is Mpox the Same as Smallpox and Chickenpox?
While Mpox, smallpox, and chickenpox share some similarities, they aren’t the same. Mpox and smallpox belong to the same virus family, Poxviridae, and both cause similar symptoms, but there are key differences. For instance, Mpox typically causes lymphadenopathy, which is the swelling of lymph nodes—a symptom not seen in smallpox. Additionally, the mortality rate for Mpox is generally lower than that of smallpox. Although they’re from different virus families, both Mpox and chickenpox can spread through close contact.

How Is Mpox Transmitted?
Mpox is primarily transmitted from animals to humans, usually through close contact with infected animals or by consuming undercooked meat from these animals. However, the virus can also spread between individuals. Human-to-human transmission occurs through prolonged skin-to-skin contact, touching surfaces or objects that have been contaminated by the virus, respiratory droplets, and even from mother to fetus or baby during childbirth. There’s also the potential for Mpox to spread through direct skin contact, although it’s still unclear if it can be transmitted via semen or vaginal fluids.
Symptoms of Mpox
The initial symptoms of Mpox are often similar to those of other viral infections, starting with fever, muscle aches, and a sore throat. What sets Mpox apart is the distinctive rash that begins on the face and gradually spreads across the body, including the palms and soles. This rash goes through several stages over a period of 2 to 4 weeks—starting as flat, red spots (macules), then becoming raised bumps (papules), before forming fluid-filled blisters (vesicles) and finally turning into pustules. Alongside the rash, typical symptoms include headache, muscle aches, swollen lymph nodes, and fever. The incubation period for the virus usually ranges from 7 to 14 days, though it can be as short as 5 days or as long as 21 days.
When to Get Tested for Mpox
If you develop symptoms like fever, swollen lymph nodes, and a rash—especially if you’ve recently traveled to an area experiencing an Mpox outbreak— get assessed for the virus. Testing typically starts with a PCR test to detect Orthopoxvirus, followed by a confirmatory test specifically for Mpox DNA.
Treatment for Mpox
There is no specific treatment for Mpox, so care is mostly supportive, focusing on managing symptoms and preventing complications. For the characteristic skin rash, applying antiseptic ointments and dressing the lesions can help, along with antibiotics if there’s a risk of secondary infections. In cases of genital ulcers, sitz baths are often recommended, while oral ulcers can be eased with salt gargling or topical gels. To prevent dehydration, fluid therapy is crucial, along with ensuring proper nutritional intake through a balanced diet. For symptom relief, medications like paracetamol can be used to reduce fever, and antiemetics can help manage nausea.
This is based on our research. Please make sure to consult your doctor before consuming any medications.
Home care for Mpox patients
If you’re managing Mpox at home, there are several important steps to take to protect yourself and others. Self-isolate as much as possible and minimize contact with others, especially if you’re experiencing respiratory symptoms. Wearing a mask can help reduce the risk of spreading the virus, and using disposable gloves, along with practicing good hand hygiene, is crucial. Make sure to clean and sanitize any contaminated surfaces and laundry regularly. It’s also wise to avoid contact with pets to prevent any potential transmission.

Is Mpox deadly?
While most Mpox infections resolve within a few weeks, complications can occur, particularly in children. These complications can include secondary infections, pneumonia, and in some cases, even death. The current estimated mortality rate is between 3-6%, with children being more vulnerable.
Vaccines that were originally developed to protect against smallpox can also offer protection against Mpox. However, since the eradication of smallpox, no new vaccines have been produced domestically. In the United States, the JYNNEOSTM vaccine is available and is licensed to protect against both Mpox and smallpox.
What next?
As Mpox continues to make its presence felt across the globe, it’s clear that this virus is more than just a passing concern. While India and many other regions have so far managed to keep the situation under control, the evolving nature of viral outbreaks reminds us how fragile our sense of normalcy can be. In a world where the lines between past pandemics and future threats blur, staying informed and prepared isn’t just a precaution—it’s a necessity.
This isn’t about fear-mongering; it’s about recognizing the reality we live in. Viruses like Mpox are part of a broader, shifting landscape of global health that demands our constant vigilance. But with the right knowledge and a commitment to public health measures, we can navigate these challenges without losing sight of what matters most: the safety and well-being of our communities.
We’re not just passive observers in this story—we’re all part of it. If you’re a writer, a storyteller, or someone passionate about the journalistic path, we want to hear from you. Whether you have personal experiences to share, or you’re eager to dive into topics like this, your voice could make a difference. Join us in exploring and reporting on the issues that shape our world, and let’s continue to shed light on the stories that matter.
Write to [email protected]
Jargon Junction
Word: Gambian Pouched Rat
Sentence within the article: “It’s caused by the Mpoxvirus, a name that reflects its history—though the virus was first discovered in monkeys back in 1958, its primary reservoirs are actually rodents like rope squirrels, tree squirrels, Gambian pouched rats, and dormice.”
What it actually is: A large rodent species native to Africa, known for its cheek pouches used to store food. These rats are significant because they can carry and transmit the Mpox virus to humans, acting as a reservoir for the disease.
Jargon Junction
Word: Sitx Baths
Sentence within the article: “In cases of genital ulcers, sitz baths are often recommended, while oral ulcers can be eased with salt gargling or topical gels.”
What it actually is: A therapeutic bath in which only the hips and buttocks are soaked in warm water. It is often used to relieve pain or discomfort in the lower part of the body, especially in cases of ulcers or other irritations caused by infections like Mpox.